You’re looking at dozens of medical images on your screen, trying to piece together what’s happening inside a patient’s body.
Multi modality imaging has become the norm in modern radiology, but managing all these different scans can feel overwhelming.
That’s where synchronized viewing comes in—a technique that can transform how you analyze complex cases.
What Makes Synchronized Viewing Different?
Think of synchronized viewing as having multiple monitors that move together.
When you scroll through one image series, all the related images move at the same time. This isn’t just convenient—it’s often essential for accurate diagnosis.
The technique works by linking different imaging modalities or time points so you can see corresponding anatomy across all views simultaneously.
Instead of jumping between separate windows, you get a unified view that shows how structures relate to each other.
Key Scenarios for Synchronized Viewing
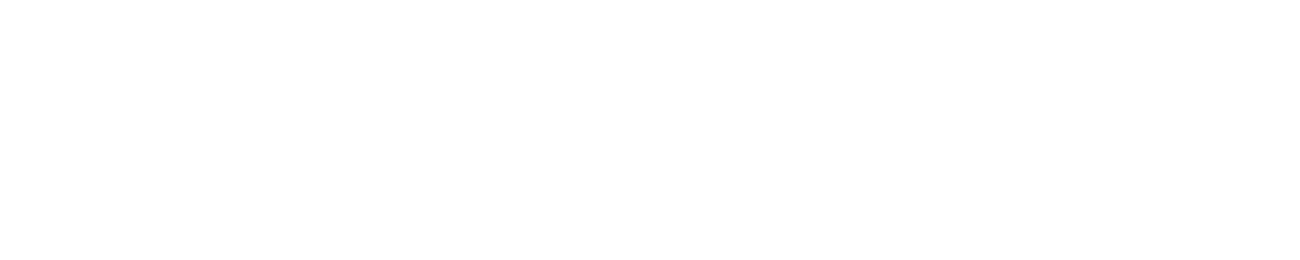
Cancer Detection and Staging
When you’re hunting for tumors, synchronized viewing becomes your best friend. You can watch how a suspicious area appears across different imaging types:
- CT and MRI correlation: See how a mass shows up on both scans
- PET-CT fusion: Watch metabolic activity align with anatomical structures
- Pre and post-contrast studies: Track how lesions enhance over time
Research shows that radiologists using synchronized viewing detect 15-20% more lesions compared to reviewing images separately. This improvement matters when you’re dealing with cancer staging or treatment planning.
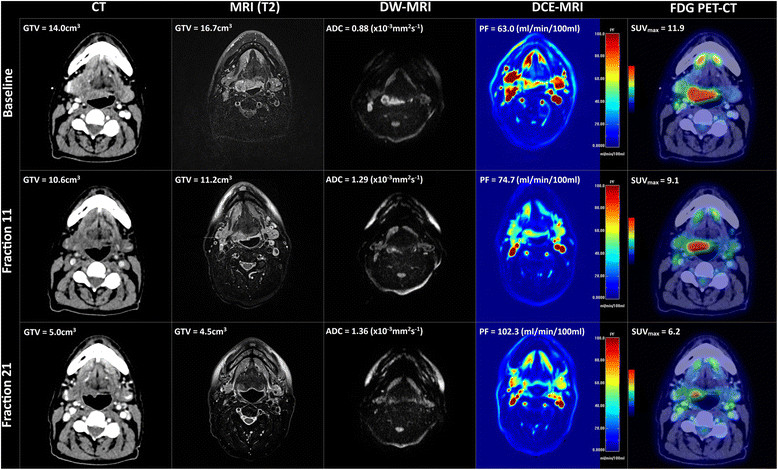
Cardiac Imaging Analysis
Your heart moves constantly, making cardiac imaging particularly challenging. Synchronized viewing helps you track:
- Wall motion across different cardiac phases
- Perfusion patterns in stress tests
- Coronary artery changes over time
Key benefit: You can spot subtle wall motion abnormalities that might be missed when viewing cine loops separately.
Neurological Assessments
Brain imaging often requires multiple sequences to tell the complete story. Synchronized viewing excels when you need to:
- Compare FLAIR and T2 images for lesion characterization
- Track stroke evolution across time points
- Correlate functional imaging with anatomical scans
Studies indicate that synchronized viewing reduces interpretation time by 30-40% for complex neurological cases.
Performance Impact: The Numbers
| Imaging Scenario | Time Savings | Accuracy Improvement |
| Multi-phase CT | 25-35% | 12-18% |
| PET-CT fusion | 40-50% | 15-22% |
| Cardiac cine | 20-30% | 8-15% |
These numbers come from real-world studies comparing synchronized versus traditional viewing methods. The time savings alone can help you handle higher case volumes without sacrificing quality.
When Not to Use Synchronized Viewing?
Sometimes synchronized viewing can actually slow you down or create confusion:
Single-modality routine studies: If you’re reading a straightforward chest X-ray or simple ultrasound, synchronized viewing adds unnecessary complexity.
Different anatomical regions: Don’t try to synchronize a brain MRI with an abdominal CT. The anatomical mismatch will confuse rather than help.
Significant patient movement: If the patient moved between scans, synchronized viewing might align images incorrectly, leading to misinterpretation.
Setting Up Your Workflow
Getting synchronized viewing to work smoothly requires some planning:
Image registration: Make sure your images are properly aligned before synchronizing. Poor registration creates more problems than it solves.
Display optimization: Use high-resolution monitors with consistent brightness. Color calibration matters more when you’re comparing multiple image types.
Software familiarity: Spend time learning your PACS system’s synchronization features. Most modern systems offer multiple sync options—find what works best for your practice.
The Future of Synchronized Viewing
Artificial intelligence is making synchronized viewing even more powerful. AI-assisted registration can automatically align images from different time points or modalities, reducing setup time.
Machine learning algorithms are also starting to highlight corresponding anatomy across different image types, making it easier to spot correlations you might miss.
Making the Switch
If you’re not using synchronized viewing regularly, start small. Pick one imaging scenario where you frequently compare multiple series—maybe contrast-enhanced CT or cardiac MRI.
Get comfortable with the workflow before expanding to more complex cases.
The learning curve is usually short, but the benefits last throughout your career.
Once you experience the efficiency and accuracy gains, you’ll wonder how you ever managed without synchronized viewing techniques for your most challenging diagnostic cases.